Let’s tackle the time-honored discussion: breastfeeding versus formula-feeding. We frequently catch ourselves contemplating the options, assessing the advantages and disadvantages of each approach.
The benefits and drawbacks of these feeding options are worth exploring, as they play an important role in shaping a baby's early development. From nutritional content to bonding experiences, the complexities of this decision are vast.
As we navigate through the worlds of nourishment for our little ones, we uncover a myriad of factors that influence our choices. So, which path will lead to the best nourishment for our baby?
Key Takeaways
- Breast milk offers unparalleled nutritional benefits and immune support.
- Formula feeding provides convenience and shared feeding responsibilities.
- Both methods promote bonding and nurturing experiences for caregivers.
- Breastfeeding has significant health advantages for both mother and baby.
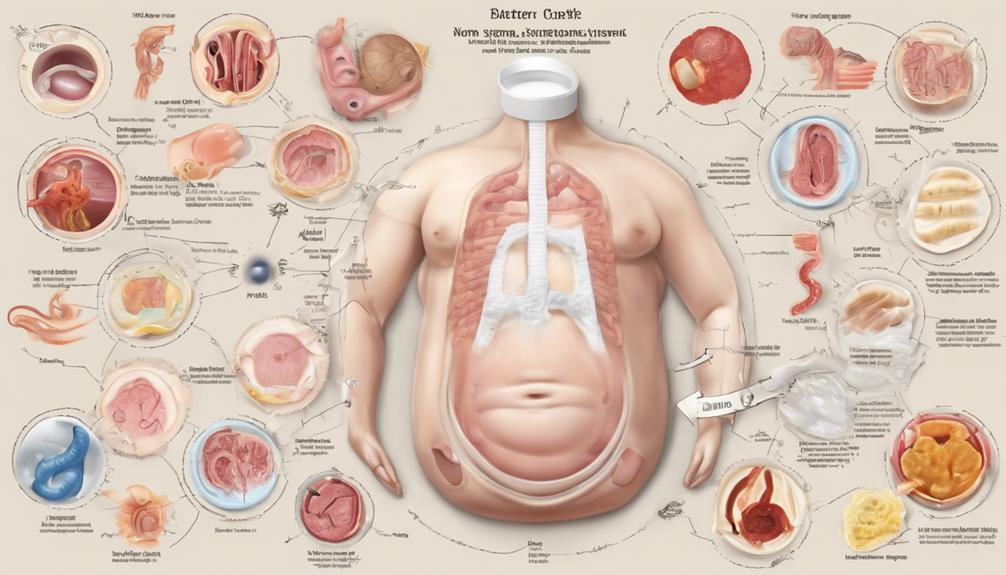
Nutritional Differences
Breast milk, with its rich assortment of antibodies, enzymes, and growth factors, provides essential nutrients important for supporting a baby's immune system and overall development. The nutritional content of breast milk is uniquely tailored to meet the evolving needs of an infant, adapting to provide the best nourishment at each developmental stage.
Unlike formula milk, breast milk offers bioactive components such as lactoferrin and oligosaccharides that play a vital role in promoting gut health, bolstering immune function, and safeguarding against infections. These components are absent in formula milk, making breast milk an unparalleled source of nutrition for infant growth and development.
While formula milk serves as a viable alternative, providing essential nutrients like proteins, carbohydrates, fats, vitamins, and minerals in a balanced form, it lacks the dynamic composition of breast milk. Manufacturers aim to mimic the nutritional content of breast milk to support infant growth and development, yet the bioactive components present in breast milk remain unmatched by formula milk.
Breastfeeding stands out as a superior choice providing essential nutrients and bioactive components important for infant health and well-being.
Feeding Convenience

When considering feeding convenience, the ability for various caregivers to feed the baby easily becomes a significant factor to weigh in the decision-making process. Formula feeding offers a range of conveniences that can simplify the feeding routine for both parents and other caregivers involved. Here's why:
- Flexibility for All: With baby formula, anyone can feed the baby, providing mothers with more flexibility in their daily schedules.
- Structured Feeding Schedule: Formula feeding allows for easier scheduling of feedings as formula isn't digested as quickly as breast milk, making it easier to plan and predict feeding times.
- Enhanced Partner Involvement: Partners can actively participate in feedings and bonding experiences, contributing to a shared responsibility and strengthening the family unit.
These aspects highlight how formula feeding can streamline the feeding process, offering convenience and shared involvement among caregivers in the nurturing journey of the baby.
Bonding and Emotional Aspects
Considering the nurturing journey of the baby, exploring the emotional connections and bonding experiences between caregivers and the infant is essential in understanding the impact of feeding choices. Breastfeeding plays a significant role in bonding as it promotes skin-to-skin contact and triggers the release of oxytocin, often referred to as the 'love hormone.' This intimate act fosters a strong maternal bond and enhances emotional connections between mother and baby.
On the other hand, formula feeding allows for partners and other caregivers to participate in feeding, creating bonding opportunities through nurturing routines and engagement during feeding sessions. While both feeding methods offer avenues for bonding, breastfeeding has been associated with lower rates of maternal postpartum depression, potentially influencing the emotional bond with the baby.
Ultimately, the emotional aspects of feeding routines play a vital role in shaping the relationship between caregivers and the infant, establishing a foundation for lifelong connections and attachment.
Health Benefits and Risks
Exploring the health benefits and risks associated with infant feeding methods reveals significant differences in long-term outcomes for both the baby and the mother. When considering breastfeeding versus formula-feeding, the health advantages are clear:
- Breast milk provides immune-boosting antibodies: Breastfed babies are better equipped to fight off infections and diseases due to the protective components present in breast milk.
- Enhanced maternal health: Mothers who breastfeed have lower rates of breast and ovarian cancer, as well as reduced risks of cardiovascular diseases compared to those who opt for formula feeding.
- Cost-effective and nutritionally superior: Breast milk is tailored to meet the baby's nutritional needs and is free of cost, unlike formula feeding which can be a significant financial burden, costing anywhere from $800 to $2,800 annually.
Choosing to breastfeed not only benefits the baby with enhanced immunity and long-term health advantages but also positively impacts the mother's well-being and saves on costs when compared to formula feeding.
Practical Considerations
Practical considerations play an important role in determining the most suitable infant feeding method for both the baby and the caregiver. While formula-feeding offers convenience by allowing caretakers to feed the infant in the absence of the mother, it can be costly in the long run and may lead to digestive issues like constipation and gas in some formula-fed babies.
On the other hand, breastfeeding, although initially requiring more frequent feedings, provides unique health benefits through the presence of immunoglobulins in breast milk that support the infant's immune system. Proper preparation and cleanliness of formula are critical to guarantee the baby's health and safety when opting for this feeding method.
Over time, breastfeeding schedules become more predictable, offering a natural and cost-effective way to feed the infant while promoting the best health. Careful consideration of these practical aspects is essential in deciding on the most suitable feeding option for the infant's well-being.
Frequently Asked Questions
Is There Really a Difference Between Breastfed and Formula-Fed Babies?
Yes, there is a difference between breastfed and formula-fed babies. Breastfeeding offers unique immune system support and health benefits not found in formula. Evidence shows breastfed babies may have lower risks of infections, allergies, and SIDS.
What Do Studies Comparing Breast Feeding With Bottle Feeding Formula Show?
Studies indicate that breastfeeding offers numerous health benefits for both baby and mother, including lower risks of infections, allergies, and respiratory illnesses. The evidence supports the importance of considering breastfeeding over formula feeding for best health outcomes.
How Is Breast Milk Composition Compared to Formula?
Breast milk, tailored to our baby's needs, offers a plethora of nutrients and immune factors that formula can't match. Its live cells and dynamic composition support our baby's health in ways formula can't replicate, making breastfeeding invaluable for us.
Is Breastfeeding More Digestible Than Formula?
Yes, breastfeeding is more digestible than formula for babies. Breast milk's tailored composition aids in easier digestion, reducing issues like constipation and gas. Its enzymes and antibodies support peak nutrition, making it easier for babies to absorb nutrients efficiently.
Conclusion
To sum up, the decision between breastfeeding and formula-feeding is a personal one that should be based on what works best for both the baby and the mother.
While both methods have their own set of benefits and challenges, ultimately, the most important thing is ensuring that the baby is well-nourished and loved.
So, whether you choose breastfeeding or formula-feeding, what matters most is the bond and care you provide to your little one.