Breastfeeding/Formula Feeding
Managing Pregnancy Symptoms While Breastfeeding
Fascinated by the challenges of juggling pregnancy symptoms and breastfeeding? Find practical tips to navigate this unique journey with ease.

Up to 75% of mothers who breastfeed report experiencing symptoms of pregnancy as they tend to their babies, facing a distinctive array of obstacles. The task of managing breastfeeding responsibilities along with the physical and emotional shifts pregnancy brings can prove to be daunting.
However, there are practical strategies and self-care tips that can be valuable in managing this complex journey. From managing fatigue and nausea to coping with mood swings, finding effective ways to address these symptoms is essential for the well-being of both the mother and the baby.
Let's explore some insightful approaches to help mothers manage this delicate balance with confidence and support.
Key Takeaways
- Adjust feeding routine to ease physical strain of pregnancy.
- Seek professional guidance for maternal and infant health optimization.
- Monitor changes in discomfort, milk supply, and complications.
- Prioritize self-care and communicate effectively with family and caregivers.
Symptoms to Expect While Breastfeeding
Experiencing various physical and emotional changes is common for breastfeeding mothers as they navigate through pregnancy symptoms while caring for their infant. Pregnancy symptoms while breastfeeding can present unique challenges.
Fatigue may be more pronounced due to the demands of both breastfeeding and early pregnancy. Sore breasts, a common symptom of both breastfeeding and pregnancy, can cause discomfort. Nausea, often associated with pregnancy, might be exacerbated while breastfeeding. Frequent urination can also increase, adding to the physical strain. Missed periods can be confusing for breastfeeding mothers, as it could indicate pregnancy. Breast tenderness, bloating, and food aversions are additional symptoms that can occur while breastfeeding and pregnant.
Keeping an eye out for these signs can help in detecting pregnancy early on. Understanding these potential symptoms is essential for managing the delicate balance of pregnancy and breastfeeding.
Balancing Pregnancy and Breastfeeding

Effectively managing the dual responsibilities of pregnancy and breastfeeding necessitates a strategic approach focused on proper nutrition, rest, and hydration for the well-being of both the mother and the developing fetus.
- Adjust Feeding Routine: Adapting the breastfeeding frequency and duration can help alleviate some of the physical demands of pregnancy while still providing essential nourishment to the baby.
- Seek Professional Support: Consulting with healthcare providers and lactation consultants can offer valuable guidance on how to optimize maternal and infant health during this unique phase of balancing pregnancy and breastfeeding.
- Monitor for Changes: Keeping a close eye on any signs of discomfort, fluctuations in milk supply, or potential complications is essential for maintaining a healthy equilibrium between the demands of pregnancy and the needs of breastfeeding.
Maintaining open communication with family members and caregivers can foster a supportive environment that caters to the requirements of both the pregnant mother and the breastfeeding child. Prioritizing self-care and seeking assistance when needed are key components of successfully sailing through the intricacies of being pregnant while continuing to breastfeed.
Managing Fatigue and Nausea
To manage fatigue and nausea while breastfeeding during pregnancy, it's essential to prioritize rest, maintain a balanced diet, and stay hydrated. Fatigue can be alleviated by ensuring you're getting enough sleep and seeking assistance with household chores. Nausea, a common pregnancy symptom, can be managed by eating small, healthy snacks throughout the day. Consider trying motion sickness wristbands for relief from nausea while breastfeeding.
Important hydration is key, and avoiding triggers like strong odors can help reduce nausea. Ensuring a balanced diet rich in nutrients is key to managing these symptoms. Remember to listen to your body's cues and take breaks when needed. By taking care of yourself and incorporating these strategies, you can better cope with fatigue and nausea while breastfeeding during pregnancy.
Coping With Mood Swings

Pregnancy and breastfeeding often bring about significant hormonal changes that can lead to emotional fluctuations, making it important to address coping mechanisms for managing mood swings effectively.
Here are three essential strategies to help you navigate through mood swings during this challenging time:
- Seek Support: Surround yourself with understanding and empathetic loved ones who can provide a listening ear and a comforting presence. Sometimes, simply talking about your feelings can alleviate the intensity of mood swings.
- Practice Self-Care: Engage in self-care practices that promote emotional well-being, such as taking short breaks for relaxation, getting sufficient rest, eating balanced meals, and staying hydrated. Prioritizing your own needs can contribute to better emotional balance.
- Consider Professional Help: If mood swings become overwhelming or interfere with your daily life, don't hesitate to seek assistance from a counselor or therapist. Professional guidance can offer valuable strategies and tools to manage mood swings effectively.
Self-Care Tips for Mothers
How can mothers prioritize self-care to support their well-being during pregnancy and breastfeeding?
Self-care is important during this time to manage symptoms, promote health, and nurture the bond with your baby. To combat fatigue and maintain milk supply, make sure proper rest and stay hydrated. Eating nutrient-dense, small meals can ease nausea and provide energy.
Seeking support from loved ones or support groups can ease emotional stress and offer practical help. Gentle exercises like walking or prenatal yoga can enhance relaxation, improve circulation, and alleviate discomfort.
Consulting healthcare providers for personalized guidance ensures the well-being of both you and your baby. Prioritizing self-care not only benefits you but also positively impacts your breastfeeding journey and overall pregnancy experience. Remember, taking care of yourself isn't selfish but essential for being the best mother you can be.
Frequently Asked Questions
Can Pregnancy Symptoms Be Different When Breastfeeding?
Pregnancy symptoms can vary when breastfeeding. Hormonal changes may alter how symptoms manifest. Fatigue, breast tenderness, and nausea can still occur. Detecting pregnancy might require keen observation. Some women may notice symptoms more intensely while breastfeeding.
What Are the Symptoms of Pregnancy for a Breastfeeding Mother?
Pregnancy symptoms for a breastfeeding mother can vary but commonly include fatigue, breast tenderness, nausea, mood swings, and more. These signs, like whispers in the wind, should prompt consulting a healthcare provider for guidance.
When Should I Take a Pregnancy Test if I Am Breastfeeding?
We suggest taking a pregnancy test after a missed period, ideally around 2 weeks post-conception. For accurate results, test in the morning when urine is concentrated. Breastfeeding may influence hormone levels, so consult a healthcare provider for guidance on timing.
How Can I Control My Pregnancy While Breastfeeding?
We juggle the demands of pregnancy and breastfeeding by adjusting routines, nourishing ourselves well, seeking expert advice, and prioritizing self-care. Balancing both journeys requires flexibility, guidance, and self-compassion to navigate successfully.
Conclusion
To sum up, managing pregnancy symptoms while breastfeeding can feel like juggling flaming torches while riding a unicycle on a tightrope.
It requires a delicate balance of self-care, support from loved ones, and guidance from healthcare professionals.
With determination, perseverance, and a sprinkle of magic, mothers can navigate through this challenging but rewarding journey with grace and strength.
Remember, you're a superhero in disguise, capable of overcoming any obstacle that comes your way.
With a rich background in writing and a keen interest in child development, she specializes in creating insightful, compassionate content that speaks directly to parents’ concerns and aspirations. Margaret believes in the power of shared experiences to bring comfort and confidence to parents everywhere.
Breastfeeding/Formula Feeding
Balancing Your Breastfeeding Diet for a Less Gassy Baby
Discover the key to relieving your baby's gas issues by balancing your breastfeeding diet – could your diet be causing discomfort?

When it comes to nourishing our little ones, we all want to make sure they're content and comfortable.
Imagine this: you're cuddling your baby, but the persistent gassiness is causing discomfort. Could your diet be a factor?
Join us as we explore the delicate balance of foods that can help ease your baby's gas issues.
Let's uncover the secrets to creating a breastfeeding diet that promotes a happy, less gassy baby.
Key Takeaways
- Incorporate probiotic-rich foods like yogurt for a healthy gut and less gas in your baby.
- Opt for easily digestible proteins such as chicken and fish to minimize gas issues.
- Maintain hydration with water-rich foods and 8-10 glasses daily for optimal breastfeeding.
- Monitor dairy intake to identify triggers for gas problems in your baby.
Foods That Reduce Baby's Gas
Moreover, incorporating probiotic-rich foods like yogurt into our breastfeeding diet can aid in reducing our baby's gas discomfort by fostering a healthy gut microbiome. When we consume foods that support a balanced gut flora, we're indirectly benefiting our breastfeeding baby by potentially decreasing excessive gas production.
Opting for easily digestible proteins such as chicken or fish can also play a significant role in minimizing gas in breastfed babies. These protein sources are gentle on the digestive system, making it easier for our little ones to process nutrients from breast milk efficiently.
Moreover, including fiber-rich foods like oats and brown rice in our diet can regulate digestion for both mom and baby, potentially decreasing the occurrence of gas. Additionally, choosing low-gas vegetables like carrots and squash over high-gas options such as broccoli and cabbage can further help alleviate baby gas. By being mindful of our food choices, we can contribute to a more comfortable feeding experience for our breastfeeding baby.
Proper Hydration for Breastfeeding Moms

To maintain peak milk production and support our baby's nourishment, breastfeeding mothers should prioritize consuming 8-10 glasses of water daily for proper hydration. Adequate fluid intake is vital for breastfeeding moms as dehydration can lead to a decrease in milk supply. Including water-rich foods like fruits and vegetables in our diet can also help maintain hydration levels.
Since breast milk is mainly water, at about 88%, staying properly hydrated is essential for both milk volume and quality. Signs of dehydration in breastfeeding moms, such as dark urine, feeling thirsty, and reduced milk production, indicate the necessity of maintaining proper hydration levels.
Balancing Protein Intake for Baby's Comfort
Balancing your baby's comfort through a well-rounded protein intake is essential for supporting their growth and development during breastfeeding. Including protein-rich foods like meat, poultry, fish, eggs, dairy, beans, nuts, and seeds in your breastfeeding mother's diet can help maintain a balanced diet for your baby's comfort.
Consuming protein 2-3 times a day is vital for adequate milk production and promoting a healthy breastfeeding experience. Variety in protein sources can reduce the likelihood of gassiness in your baby.
Balancing protein intake with other essential nutrients can lead to a less gassy and more comfortable breastfeeding experience for your baby. If your baby experiences tummy troubles, consider consulting a lactation consultant to evaluate your diet. Remember that some babies might've sensitivities to certain proteins, so if you suspect a food allergy, an elimination diet might be necessary.
Be mindful of dairy products and other common allergens in your diet to alleviate potential discomfort for your baby.
Importance of Fiber in Breastfeeding Diet
Fiber plays a critical role in supporting digestion and preventing constipation for both breastfeeding mothers and their babies. Adequate fiber intake is essential for maintaining a healthy gut microbiome, which can positively impact the baby's digestive system. Incorporating fiber-rich foods like fruits, vegetables, whole grains, and legumes into a breastfeeding diet not only provides important nutrients for the mother but can also benefit the breastfed baby's digestive health.
High-fiber foods contribute to a feeling of fullness, aiding in postpartum weight management for mothers. It's important to consume a variety of fiber sources to make sure a well-rounded and nutritious breastfeeding diet. By focusing on fiber-rich foods, breastfeeding mothers can support their own digestive health while potentially reducing gas and digestive issues in their breastfed babies. Prioritizing fiber in the breastfeeding diet can lead to overall better health outcomes for both mother and baby.
Monitoring Dairy Consumption for Gas Relief
When considering the management of gas relief in breastfed babies, it's important to monitor dairy consumption for potential triggers. Dairy products like milk, cheese, and yogurt can often be the culprits behind gas issues in breastfed infants.
Here are some key points to bear in mind when monitoring dairy intake for gas relief:
- Dairy Allergies: Approximately 2-3% of breastfed babies may have true allergic reactions to dairy in the mother's diet, causing excessive gas.
- Symptoms to Watch for: Signs of dairy sensitivity in babies include colic, gas, fussiness, or changes in stool consistency.
- Elimination Approach: Eliminating dairy from the mother's diet has been shown to help alleviate gas symptoms in some breastfed babies.
- Consult Healthcare Provider: Before making significant dietary changes to address gas issues in breastfed infants, it's vital to consult a healthcare provider for proper guidance and monitoring.
Frequently Asked Questions
Is My Breastfed Baby Gassy Because of My Diet?
Yes, our breastfed baby may be gassy due to our diet. Some foods like dairy, broccoli, and garlic can cause gas in babies. Eliminating these foods or seeking guidance from a healthcare provider can help ease baby's discomfort.
How Can I Make My Breast Milk Less Gassy?
We can make breast milk less gassy by avoiding gas-inducing foods like broccoli, cabbage, and beans. Dairy, eggs, wheat, peanuts, soy, fish, and nuts can also cause gas in babies. Consulting a healthcare provider for guidance is important.
What Foods Cause Upset Stomach in Breastfed Babies?
We've learned that dairy, eggs, wheat, peanuts, soy, fish, nuts, and certain veggies like broccoli can upset a breastfed baby's stomach. Being mindful of these foods can help ease digestive issues and guarantee a happier baby.
Why Is My Breastfed Baby Struggling With Gas?
We found that breastfed babies may struggle with gas due to air swallowing or foods in the mother's diet passing into breast milk. Monitoring diet and consulting a healthcare provider can help manage and reduce gas in babies.
Conclusion
Just as a well-balanced diet is key to reducing gas in our babies, so too is finding harmony in our own lives. By nourishing ourselves with the right foods and staying hydrated, we can create a peaceful environment for our little ones to thrive.
Remember, just as we feed our babies with love and care, we must also care for ourselves with the same intention. Balancing our diet isn't just about food, but about finding balance in all aspects of our lives.
With a rich background in writing and a keen interest in child development, she specializes in creating insightful, compassionate content that speaks directly to parents’ concerns and aspirations. Margaret believes in the power of shared experiences to bring comfort and confidence to parents everywhere.
Breastfeeding/Formula Feeding
Top Non-Dairy Tube Feeding Formulas for Sensitive Individuals
Trek through the realm of non-dairy tube feeding formulas for sensitive individuals to uncover transformative solutions that defy expectations.

When venturing into the realm of non-dairy tube feeding formulas for those with sensitivities, it can feel like trying to find a needle in a haystack – a meticulous and careful endeavor.
As we investigate the landscape of options available, there are key contenders like Liquid Hope that stand out for their dedication to providing nourishment without dairy-based ingredients.
However, the journey doesn't stop here. What other hidden gems might await discovery in the world of non-dairy tube feeding formulas, promising both efficacy and sensitivity to individual needs?
Stay tuned for insights into top choices that could revolutionize tube feeding for the dairy-sensitive.
Key Takeaways
- Liquid Hope, Kate Farms, Real Food Blends, and Functional Formularies offer dairy-free tube feeding options.
- These formulas are free from gluten, soy, and corn, catering to sensitive individuals' dietary needs.
- Provide essential nutrients with 450 calories per serving for optimal nutrition without lactose intolerance discomfort.
- Choose plant-based, organic, and natural ingredients to support gentle digestion and overall well-being.
Liquid Hope Organic Whole Foods Formula
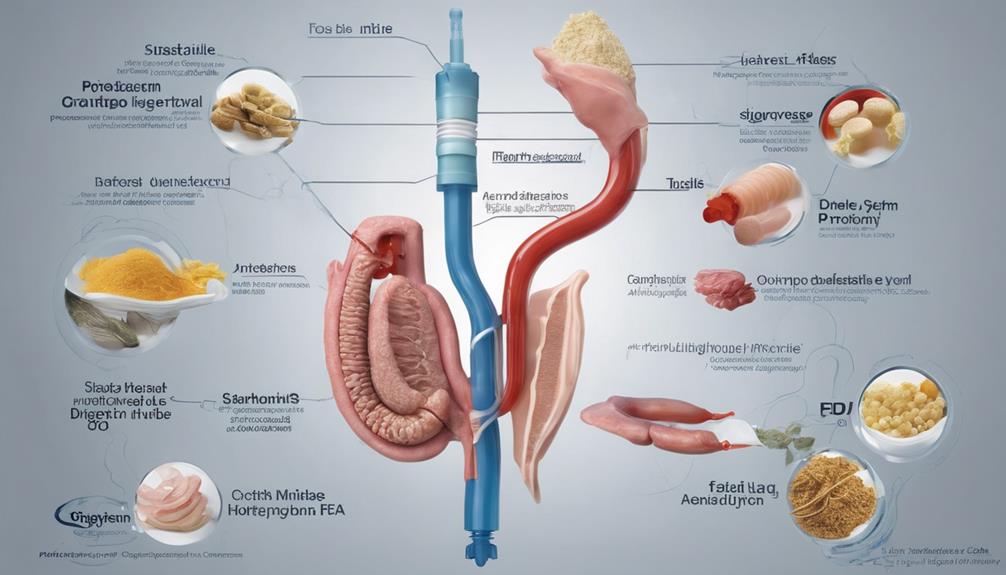
Liquid Hope Organic Whole Foods Formula is a shelf-stable, USDA Certified Organic, plant-based formula designed for individuals requiring tube feeding or seeking a nutritious oral option. With 450 calories and 9g of dietary fiber per serving in a 12 oz pouch, Liquid Hope offers a convenient and nutrient-dense choice.
This formula caters to those with lactose intolerance, providing a well-rounded nutrition source that supports weight maintenance and the body's natural immune function. The emphasis on whole foods and the absence of common allergens like gluten, dairy, soy, and corn make Liquid Hope ideal for sensitive individuals looking to enhance their daily organic nutrient intake.
Its extended 2-year shelf life aligns with a food-as-medicine approach, ensuring a reliable and effective option for those in need of increased organic nutrients without compromising on quality or taste.
Kate Farms Nutrition Options

Among the diverse range of organic, non-dairy tube feeding formulas available, Kate Farms Nutrition Options stand out for their plant-based, USDA Certified Organic, and GMO-free compositions tailored to accommodate individuals with specific dietary needs.
Kate Farms offers a variety of high-calorie, fiber-rich options such as Essential 1.2 and Peptide, designed to meet the nutritional requirements of sensitive individuals reliant on tube feeding. These formulas, like Kate Farms Peptide, provide essential nutrients without common allergens like gluten, dairy, soy, and corn, supporting overall health and well-being.
The emphasis on being plant-based guarantees gentle digestion, making them ideal for those with sensitivities. The USDA Certified Organic certification guarantees the use of organic ingredients, while being GMO-free ensures the formulas are free from genetically modified organisms.
Kate Farms Nutrition Options are crafted to deliver optimized nutrition for individuals with specific dietary restrictions, offering a complete solution for those in need of specialized tube feeding formulas.
Real Food Blends Tube Feeding
Kate Farms Nutrition Options cater to specific dietary needs. Moving to the discussion of Real Food Blends Tube Feeding, it's important to mention that Real Food Blends offers real food-based tube feeding formulas made with whole ingredients for individuals requiring gentle and natural nutrition options.
When considering Real Food Blends for individuals with dietary sensitivities, several key points stand out:
- Whole Foods Feeding Tube: Real Food Blends tube feeding formulas consist of real, whole ingredients, ensuring a more natural approach to tube feeding.
- Easy Digestion: These blends are designed for easy digestion, making them suitable for individuals with sensitive stomachs or those seeking gentle nutrition options.
- Diverse Meal Options: Real Food Blends offers a variety of flavors and meal options, catering to diverse nutritional needs and preferences for tube feeding.
Real Food Blends stands out for its commitment to providing tube feeding formulas that prioritize natural ingredients, easy digestion, and a range of meal choices to support individuals with unique dietary requirements.
Functional Formularies Nourishment

Functional Formularies Nourishment presents a holistic organic feeding tube solution crafted specifically for individuals with dietary sensitivities, offering a plant-based, dairy-free, and gluten-free option rich in whole foods and essential nutrients.
Liquid Hope by Functional Formularies is a tube feeding formula that stands out for its real food ingredients, making it a nourishing choice for those requiring non-dairy tube feeding solutions. This plant-based formula isn't only dairy-free and gluten-free but also free from soy, corn, and added sugars, catering to a wide range of sensitivities.
With each 12 oz pouch providing 450 calories, this USDA Certified Organic formula guarantees individuals receive essential nutrients. Suitable for G-tube/PEG/J-tube use and compatible with enteral pumps, Functional Formularies Nourishment offers a nutritionally complete option tested down to 8 French NG tubes, providing a convenient and wholesome feeding solution for those with unique dietary needs.
Nutritional Options for Sensitive Individuals
For individuals with sensitivities or allergies to dairy products, exploring nutritional options that cater to these specific needs is essential for maintaining peak health and well-being. When considering non-dairy tube feeding formulas, it's important to choose options that aren't only dairy-free but also provide essential nutrients for overall health.
Here are three top choices for sensitive individuals:
- Liquid Hope: This plant-based, organic, and whole foods tube feeding formula offers a holistic approach to nutrition, ensuring individuals receive a well-rounded meal replacement without dairy ingredients.
- Kate Farms: Known for their Peptide formula, Kate Farms provides a dairy-free, gluten-free, and soy-free option for individuals with sensitivities. This formula is designed to meet the nutritional needs of sensitive individuals while being gentle on the digestive system.
- Non-Dairy Formulas for Lactose Intolerance: Ideal for those with lactose intolerance or dairy allergies, non-dairy tube feeding formulas offer a safe and effective alternative to traditional dairy-based options, ensuring proper nutrition without causing discomfort.
Frequently Asked Questions
What Is the Hypoallergenic Formula for Tube Feeding?
We've identified a hypoallergenic formula for tube feeding that caters to sensitive individuals.
This specialized formula is crafted without common allergens like dairy, soy, gluten, and corn. By excluding these triggers, it supports those with food sensitivities.
The aim is to provide essential nutrition without causing allergic responses, ensuring that even individuals with lactose intolerance or other sensitivities can benefit from this option.
What Are the Most Common Tube Feeding Formulas?
We've explored various tube feeding formulas, including Neocate, Elecare, Essential 1.2, Optimental 1.0, Peptamen, and Kate Farms Peptide. These options cater to different needs like allergies, nutritional balance, and digestive health.
It's essential to ponder discontinued formulas like Optimental for historical context. Each formula serves a unique purpose, highlighting the importance of choosing the right one based on individual sensitivities and requirements.
What Is the Low Calorie Enteral Formula?
We've got the scoop on the low-calorie enteral formula you're looking for.
It's specially designed to provide essential nutrients in a reduced calorie format, perfect for those needing controlled caloric intake.
Ideal for sensitive individuals, this formula offers a balanced nutritional profile without excess calories.
It's all about supporting health and well-being without compromising on essential nutrition.
This formula is a game-changer for those with specific dietary needs.
What Is the Tube Feed for Milk Free?
When it comes to tube feeding without dairy, our team comprehends the importance of finding the right formula.
Our team has researched extensively to provide you with valuable insights.
One aspect worth noting is the rise in demand for milk-free tube feeds due to the increasing prevalence of dairy allergies.
This trend highlights the critical need for effective non-dairy options to guarantee nutrition for sensitive individuals.
Conclusion
To summarize, for individuals with sensitivity to dairy, choosing the right non-dairy tube feeding formula is crucial. Liquid Hope, with its organic whole food ingredients, is a top choice for those looking for a gentle and high-quality option.
For instance, Sarah, a patient with lactose intolerance, noticed better digestion and higher energy levels after transitioning to Liquid Hope.
It's vital to consult with a healthcare provider to identify the optimal non-dairy tube feeding formula for personal requirements.
With over a decade of experience in editorial leadership, Esther has been at the helm of Mother Baby Kids since its inception. Her journey into parenting content was inspired by her own experiences as a mother, navigating the joys and challenges with a desire to support other parents. Esther is passionate about storytelling that connects, educates, and empowers families from all walks of life.
Breastfeeding/Formula Feeding
What Makes a High Calorie Feeding Tube Formula Effective?
A deep dive into the factors behind effective high-calorie feeding tube formulas will change how you view nutritional support in hospitals.
When examining the components that contribute to an effective high-calorie tube feeding formula, it’s fascinating to note that nearly one-fourth of patients in hospitals might need support with enteral nutrition during their hospitalization.
But what exactly contributes to the effectiveness of these specialized formulas? The answer lies in a complex interplay of factors, from the nutrient content and digestibility to the caloric density and customization of the formula.
Join us as we uncover the key elements that guarantee these high-calorie feeding tube formulas truly meet the nutritional needs of patients in a profound way.
Key Takeaways
- Premium ingredients, like hydrolyzed collagen and MCTs, enhance nutrient absorption for critically ill patients.
- Customization addresses specific nutritional needs, aiding in combating deficiencies and improving outcomes.
- Balancing caloric density optimizes energy provision while minimizing risks like overfeeding and GI discomfort.
- Diverse fatty acid profiles, such as omega-3 and omega-6, support health, inflammation reduction, and heart function.
Nutrient Content Considerations
When considering nutrient content in high calorie feeding tube formulas, it's essential to focus on the concentrated macronutrients and micronutrients provided to meet specific nutritional needs.
Fatty acids, a critical component of these formulas, play a vital role in energy provision and overall health. High calorie formulas often contain a blend of saturated, monounsaturated, and polyunsaturated fats to support various bodily functions.
Polyunsaturated fatty acids, such as omega-3 and omega-6, are particularly beneficial for reducing inflammation and supporting heart health. These essential fatty acids are necessary for proper cell function and can't be produced by the body, emphasizing their importance in high calorie feeding tube formulas.
By including a diverse range of fatty acids in these formulas, healthcare providers can ensure that patients receive well-rounded nutrition that supports their unique dietary requirements.
It's crucial to consider the types and amounts of fatty acids present in high calorie formulas to optimize patient outcomes and promote overall well-being.
Digestibility Factors to Consider
Considering the digestibility factors in high calorie feeding tube formulas is paramount for ensuring efficient nutrient absorption and supporting overall patient well-being. When evaluating the digestibility of these formulas, several key factors should be taken into account:
- Inclusion of Medium-Chain Triglycerides (MCTs): MCTs are easily digestible fats that provide a quick source of energy for patients, especially those with gastrointestinal issues that may compromise fat absorption.
- Hydrolyzed Collagen Content: The presence of hydrolyzed collagen aids in digestion and absorption of essential amino acids, important for protein synthesis and tissue repair.
- Utilization of Whey Protein: Whey protein, known for its high-quality amino acid profile, supports easy digestion and utilization by the body, promoting muscle growth and overall recovery.
- Enhanced Nutrient Absorption: Effective high calorie formulas are formulated to promote best nutrient absorption in patients with compromised gastrointestinal function, ensuring that patients receive the necessary nutrients for their well-being and recovery.
Importance of Ingredient Quality
Optimizing the quality of ingredients in high-calorie feeding tube formulas is essential for maximizing nutrient absorption and supporting diverse patient needs, particularly critically ill patients. The ingredients used greatly impact the digestibility, tolerance, and overall effectiveness of the formula in meeting the nutritional requirements of these patients. For critically ill individuals, whose nutrient needs are often elevated due to their condition, high-quality ingredients play a crucial role in ensuring that the body can efficiently utilize the nutrients provided.
Premium ingredients such as hydrolyzed collagen, medium-chain triglycerides (MCTs), and whey protein not only enhance the nutritional profile of the formula but also contribute to better patient outcomes. The sourcing and composition of these ingredients are critical factors that influence the formula's efficacy in delivering essential nutrients to individuals who may have compromised digestive systems or increased nutrient demands. By prioritizing ingredient quality, healthcare providers can better support the unique nutritional needs of critically ill patients through high-calorie feeding tube formulas.
Role of Caloric Density

Increasing the caloric density of feeding tube formulas is essential for providing enhanced energy delivery in a more concentrated form to meet the nutritional requirements of patients with limited gastrointestinal capacity. When considering the role of caloric density in high-calorie feeding tube formulas, there are both pros and cons to keep in mind:
- Pros:
- More Energy in Smaller Volume: Higher caloric density allows for increased energy provision without the need for large volumes, which can benefit patients with restricted fluid intake.
- Meeting Nutrient Needs: Caloric density plays a critical role in ensuring that patients receive essential nutrients even with limited intake capacity.
- Cons:
- Risk of Overfeeding: The concentrated nature of high-calorie formulas may pose a risk of overfeeding if not carefully monitored.
- Potential for GI Distress: Some patients may experience gastrointestinal discomfort or intolerance to highly concentrated formulas.
Balancing these factors is vital in optimizing feeding tube formulas to meet the specific needs of each patient effectively.
Impact of Formula Customization
When customizing high-calorie feeding tube formulas, healthcare providers can tailor nutritional content to meet the specific needs of individual patients, optimizing their recovery and overall health.
This customization is important as it allows for adjustments that address possible causes of malnutrition, such as unique dietary restrictions, preferences, or metabolic demands. By fine-tuning the calorie and protein content, specialized formulas can effectively combat specific nutrient deficiencies in critically ill patients.
For instance, patients with conditions like diabetes may require formulas that are lower in simple sugars but higher in healthy fats to manage blood sugar levels effectively. Additionally, individuals with digestive disorders might benefit from formulas that are easier to digest, reducing the likelihood of gastrointestinal discomfort.
Frequently Asked Questions
How Do You Increase Calories in Tube Feeding?
We increase calories in tube feeding by using high-calorie formulas tailored for enteral nutrition therapy. These formulas offer concentrated nutrition to support patients needing extra caloric intake.
By adjusting the caloric density of the formulas, we can meet the energy needs of patients with higher calorie requirements.
This approach is vital for addressing malnutrition and aiding patients with limited oral intake.
What Is Calorie Dense Tube Feeding Formula?
Calorie dense tube feeding formulas pack more energy into less liquid volume, ideal for patients needing high caloric intake or those with limited feeding capacity. These formulas efficiently deliver essential nutrients, vitamins, and minerals to support patients' nutritional needs.
When choosing a formula, consider individual requirements, medical conditions, and dietary goals. How can these formulas benefit patients with different needs and conditions?
How Many Calories Can You Eat in a Feeding Tube?
We can adjust the caloric intake from a feeding tube based on individual needs and goals. The amount can range from 1,200 to 2,000 calories per day.
Tailoring feeding tube formulas to deliver specific calorie amounts is essential for meeting nutritional requirements. Higher calorie formulas are particularly beneficial for patients with increased energy needs.
The caloric content of these formulas plays a critical role in supporting patients who can't eat orally.
How Do You Determine Calorie and Protein Needs for the Tube Feeding Patient?
When determining calorie and protein needs for tube feeding patients, we consider factors like age, weight, activity level, and medical condition. Protein requirements can vary from 1.0 to 2.0 grams per kilogram of body weight per day.
Accurate calculations are essential to prevent malnutrition and promote healing. Collaboration with a healthcare provider or dietitian helps set personalized goals for best nutrition support.
Conclusion
To sum up, finding the right high-calorie feeding tube formula is vital for supporting a patient's nutritional needs. By considering nutrient content, digestibility, ingredient quality, caloric density, and customization, healthcare providers can tailor a formula to optimize outcomes.
Remember, it's not just about the calories, but the quality and balance of nutrients that make all the difference in the patient's health and well-being. So, let's make sure we choose the formula that's the whole enchilada for our patients' nutritional requirements.
With over a decade of experience in editorial leadership, Esther has been at the helm of Mother Baby Kids since its inception. Her journey into parenting content was inspired by her own experiences as a mother, navigating the joys and challenges with a desire to support other parents. Esther is passionate about storytelling that connects, educates, and empowers families from all walks of life.
-

 Third Trimester4 weeks ago
Third Trimester4 weeks agoSafe Third Trimester Exercise Guide for Moms-to-Be
-

 Third Trimester1 month ago
Third Trimester1 month agoManaging Nausea in the Third Trimester: A How-To Guide
-

 Breastfeeding/Formula Feeding2 weeks ago
Breastfeeding/Formula Feeding2 weeks agoOvercoming Formula Feeding Guilt: 10 Ways to Feel Empowered
-

 Breastfeeding/Formula Feeding2 months ago
Breastfeeding/Formula Feeding2 months agoDairy-Free Breastfeeding Diet: A Comprehensive Guide
-

 Newborn Care4 weeks ago
Newborn Care4 weeks agoEssential Newborn Care: A How-To Guide for Parents
-
 First Trimester2 weeks ago
First Trimester2 weeks agoDramamine Use in Pregnancy: First Trimester Guide
-

 Third Trimester2 months ago
Third Trimester2 months agoWhat Causes Low Platelets in Pregnancy During the Third Trimester?
-

 Third Trimester2 months ago
Third Trimester2 months agoSigns of Baby Distress in Third Trimester: What to Watch For











