In the world of pregnancy experiences, the topic of brown discharge in the second trimester might seem like a mystery wrapped in secrecy. While we are aware of the typical causes such as hormonal changes, increased blood circulation, or innocuous activities causing worry, is there more to this situation than meets the eye?
Stay tuned as we unravel the layers of this intriguing pregnancy puzzle, shedding light on the potential causes and implications that might surprise even the most seasoned parents-to-be.
Key Takeaways
- Hormonal fluctuations and increased blood flow are common causes.
- Implantation bleeding and hormonal changes result in light brown discharge.
- Cervical changes, vaginal infections, and sensitivity contribute to brown discharge.
- Old blood expulsion and miscarriage risk require immediate medical attention.
Common Causes of Brown Discharge
Brown discharge in the second trimester of pregnancy can have various common causes, including hormonal fluctuations and increased blood flow to the cervix. Hormonal changes during pregnancy can lead to this type of discharge. Additionally, the increased blood flow to the cervix can cause irritation, resulting in the appearance of brown discharge. Activities such as sex or a pelvic exam can also trigger cervix irritation, leading to this phenomenon.
While brown discharge is often important, in some cases, it can signify more serious issues like preterm labor or placental problems such as placenta previa. Losing the mucous plug or experiencing a bloody show during the second trimester might indicate that labor is on the horizon. It's vital to seek advice from a healthcare provider if experiencing persistent brown discharge during this stage of pregnancy to rule out any potential complications. Remember, staying informed and seeking guidance can help guarantee a healthy pregnancy journey.
Implantation Bleeding and Hormonal Changes
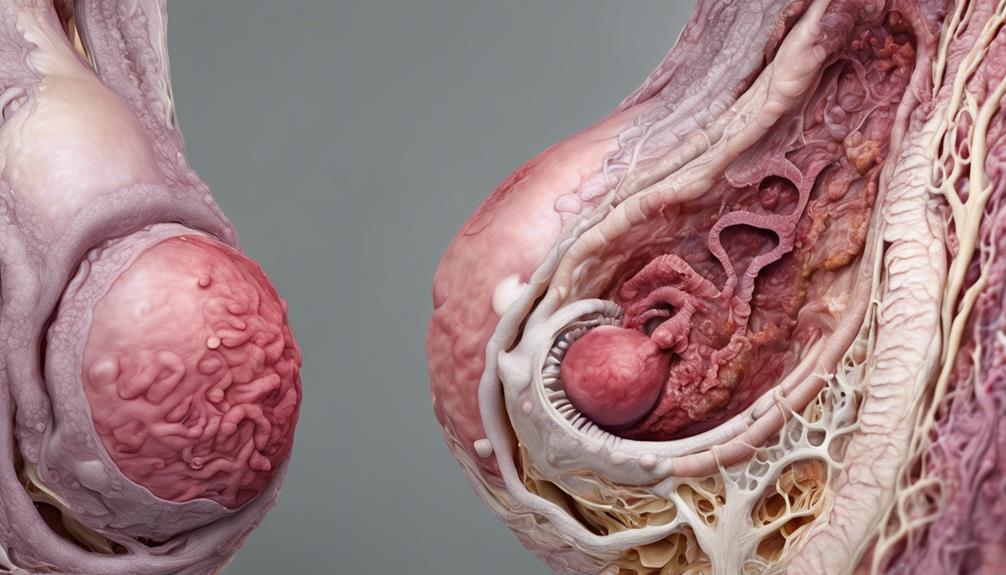
Implantation bleeding in the second trimester can result in light brown discharge as the embryo attaches to the uterine lining. Hormonal changes during this trimester can lead to increased vaginal discharge, sometimes appearing as brown discharge. The body's adjustment to pregnancy hormones may cause this occurrence. Additionally, increased blood flow to the cervix in the second trimester can make it more sensitive, occasionally resulting in brown discharge.
It is important to monitor any changes in brown discharge during the second trimester to guarantee the health of the pregnancy. While implantation bleeding and hormonal shifts can lead to brown discharge, persistent, heavy, or accompanied by other symptoms like pain or fever, medical advice should be sought promptly. Keeping track of these changes and discussing them with healthcare providers can offer reassurance and help in maintaining the well-being of both the mother and the developing baby.
Cervical Changes and Vaginal Infections
Cervical changes in the second trimester of pregnancy, influenced by increased blood flow and hormonal shifts, can contribute to the occurrence of brown discharge. Hormonal fluctuations make the cervix more sensitive, leading to occasional brown discharge. Additionally, vaginal infections such as bacterial vaginosis can play a role in causing brown discharge during this stage of pregnancy. Changes in vaginal pH levels during gestation can make pregnant individuals more prone to infections that manifest as brown discharge. Monitoring vaginal odor, itchiness, and consistency becomes essential in identifying and addressing potential vaginal infections that may result in brown discharge. To further understand the interplay between cervical changes and vaginal infections during the second trimester, let's explore the details through the table below:
| Aspect | Influence |
|---|---|
| Hormonal Fluctuations | Increase cervix sensitivity, leading to brown discharge |
| Bacterial Vaginosis | Can contribute to brown discharge through vaginal pH level changes |
| Vaginal Odor | May indicate infections causing brown discharge |
| Itchiness | Possible symptom of vaginal infections during this trimester |
| Consistency | Changes in consistency may signal underlying vaginal infections |
Old Blood Expulsion and Miscarriage Risk
During the second trimester of pregnancy, the presence of brown discharge may suggest the expulsion of old blood from the uterus, potentially indicating a risk of miscarriage if accompanied by specific symptoms. While old blood in the discharge can give it a brown color due to its age, it's generally not an immediate cause for concern.
However, it's important to pay attention to other symptoms like cramping, back pain, or heavy discharge, as these could signal a more serious issue. Monitoring the consistency and amount of brown discharge, along with any associated symptoms, is essential to determine the need for medical evaluation.
If you experience persistent or heavy brown discharge during the second trimester, seeking prompt medical attention is crucial for proper assessment and care. Remember, staying informed and proactive about any changes or symptoms you notice can help guarantee the well-being of both you and your baby during this critical stage of pregnancy.
When to Seek Medical Advice
If experiencing brown discharge with symptoms like abdominal pain, cramping, or back pain during the second trimester of pregnancy, it's important to seek medical advice promptly. Contact a healthcare provider promptly if brown discharge is accompanied by any of the following:
- Bright red spotting
- Gray discharge
- A strong odor
Immediate medical attention is necessary if brown discharge is persistent, increases in volume, or is associated with severe nausea, vomiting, or shoulder pain. It's essential to mention any changes in brown discharge to your doctor, especially if it becomes heavier, darker, or is mixed with blood clots.
Consulting a healthcare provider for any concerning signs or symptoms related to brown discharge in the second trimester is vital for proper evaluation and management. Your healthcare provider is there to support you through any uncertainties or complications that may arise during this special time.
Frequently Asked Questions
Is It Normal to Have Brown Discharge in the Second Trimester of Pregnancy?
Yes, it's common to experience brown discharge in the second trimester of pregnancy. Hormonal shifts and increased blood flow to the cervix are typical causes. Always inform your healthcare provider about any unusual discharge for proper evaluation.
When Should I Be Concerned About Discharge in Second Trimester?
If you notice any changes in discharge during the second trimester, it's important to communicate with your healthcare provider. Prompt action guarantees the well-being of both you and your baby. Trust your instincts and seek medical advice when needed.
What Should I Do if I Have Brown Discharge at 8 Weeks Pregnant?
When we faced brown discharge at 8 weeks pregnant, we reached out to our healthcare provider immediately. It's important to communicate any unusual changes for proper assessment and guidance. Trust your instincts and seek help promptly.
Is Brown Discharge Normal at 4 Weeks Pregnant?
At 4 weeks pregnant, brown discharge can be normal, often due to implantation bleeding or hormonal changes. If minimal, painless, and stable, it usually isn't concerning. However, always consult a healthcare provider for evaluation and guidance.
Conclusion
To sum up, brown discharge during the second trimester of pregnancy can be caused by various factors, including hormonal changes and cervical irritation.
It's important to monitor any changes in discharge and seek medical advice if there are concerning symptoms.
Remember, pregnancy is a journey full of twists and turns, so it's always better to be safe than sorry.
As the saying goes, 'better safe than sorry,' so trust your instincts and consult your healthcare provider for peace of mind.










