As healthcare professionals, we comprehend the concerns surrounding the use of Toradol while breastfeeding. The possible risks to infants can be a cause for concern for many. However, there are five key insights that can provide clarity on this topic and help you make informed decisions.
From its impact on milk supply to alternative options available, exploring these aspects can guide you in managing the complexities of Toradol use while nursing.
Key Takeaways
- Toradol is now contraindicated for breastfeeding due to prostaglandin effects.
- Toradol is unlikely to affect milk supply based on limited evidence.
- Consider alternative medications to avoid potential risks for babies.
- Consult healthcare provider for safe pain management options while breastfeeding.
Toradol Safety for Nursing Mothers
Toradol, despite being categorized as L2 for breastfeeding mothers, is now considered contraindicated by anesthesia and OB departments due to its prostaglandin effects. While Toradol has been known for its efficacy in post-operative pain relief for nursing mothers, recent caution has emerged regarding its safety during breastfeeding.
The prostaglandin effects of Toradol raise concerns about its impact on nursing infants, leading to a shift in recommendations against its use in lactating women. Manufacturers and current research advise healthcare providers to exercise caution when considering Toradol for nursing mothers due to potential risks involved.
Similar to the concerns raised for other NSAIDs like Motrin, the prostaglandin effects of Toradol are now under scrutiny in the context of breastfeeding. As healthcare providers, it's pivotal to prioritize the safety of both mothers and infants, necessitating a closer evaluation of Toradol's safety profile for nursing mothers.
Impact on Milk Supply
Although Toradol isn't known to impact milk supply in breastfeeding mothers, studies haven't reported any direct effects on milk production or lactation. This means that breastfeeding moms using Toradol typically don't experience a decrease in milk supply.
Here are three key points to take into account regarding Toradol and its effects on milk supply:
- Limited Evidence: While there's limited evidence on the impact of ketorolac (Toradol) on breast milk production, current research suggests that it's unlikely to have a notable effect on milk supply in breastfeeding mothers.
- Consistent Milk Production: Breastfeeding mothers who require Toradol for pain management can generally continue nursing without worrying about a significant decrease in their milk production or lactation.
- Reassurance for Breastfeeding Moms: Breastfeeding moms can find reassurance in the fact that Toradol isn't typically associated with causing a reduction in milk supply, allowing them to manage their pain while continuing to breastfeed their baby.
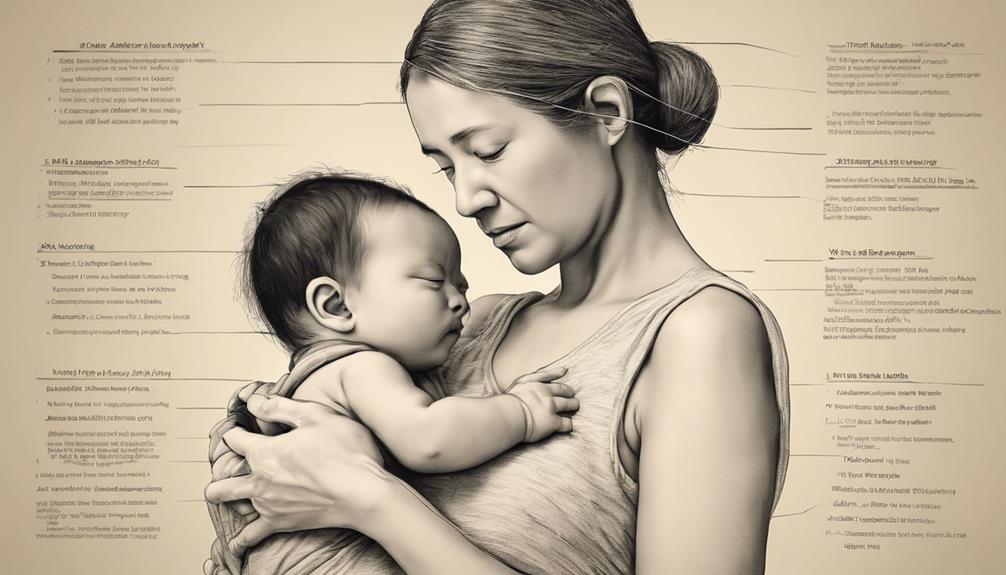
Potential Risks for Babies
Potential risks for babies when breastfeeding mothers use Toradol are influenced by factors such as the drug's transfer into breast milk and its potential effects on newborns. While ketorolac levels in breast milk are generally important with typical oral dosages, there's limited information available regarding levels after higher doses like injections or nasal sprays.
Some hospitals administer ketorolac injections post-cesarean section without reported harm to nursing infants; however, the drug's potent antiplatelet activity has led the manufacturer to advise against its use during breastfeeding. It's essential to contemplate alternative medications within the first 24 to 72 hours postpartum, especially for newborns, to avoid any potential adverse effects in breastfed infants.
When weighing the decision to use Toradol while breastfeeding, consulting healthcare providers for personalized recommendations and monitoring for any signs of complications in the baby is crucial to guarantee the safety and well-being of both mother and child.
Alternatives to Toradol
When exploring pain management options while breastfeeding, it's essential to contemplate alternative medications that are safe for both the mother and the baby. Here are some alternatives to ponder:
- Acetaminophen (Tylenol) and Ibuprofen (Advil): These over-the-counter medications can help alleviate mild to moderate pain without posing significant risks to breastfeeding infants.
- Non-pharmacological Alternatives: Non-medicinal approaches such as heat therapy, cold therapy, and relaxation techniques can be effective in managing pain while breastfeeding, providing natural relief without the use of drugs.
- Physical Therapy, Chiropractic Care, and Acupuncture: These alternative treatments offer drug-free pain management options that can be beneficial for breastfeeding mothers. They focus on addressing the root cause of pain through physical manipulation and holistic approaches.
Considering these alternatives can help mothers find safe and effective ways to manage pain while breastfeeding, ensuring the well-being of both themselves and their infants.
Consultation With Healthcare Provider
Exploring the use of Toradol while breastfeeding necessitates seeking guidance from a healthcare provider to guarantee the safety and well-being of both the mother and the baby. When consulting with a healthcare provider about Toradol and breastfeeding, it is crucial to consider individual risks and benefits to make informed decisions. Healthcare providers can offer personalized guidance and discuss potential alternatives to Toradol to ensure effective pain management while breastfeeding. Additionally, they can provide valuable information on monitoring for any potential side effects or interactions that may arise when using Toradol during breastfeeding. Seeking guidance from a healthcare provider is essential to address any concerns or questions regarding the use of Toradol while breastfeeding. This collaborative approach can help mothers navigate the complexities of pain management during breastfeeding and make choices that prioritize the health of both themselves and their babies.
| Key Points | Details |
|---|---|
| Individual Risks and Benefits | Assess personalized risks and benefits with healthcare provider. |
| Potential Alternatives | Discuss alternative pain management options suitable for breastfeeding mothers. |
| Monitoring for Side Effects | Receive guidance on monitoring and managing potential side effects. |
| Seeking Guidance | Consult healthcare provider to address concerns and make informed decisions. |
| Informed Decisions | Collaborate with healthcare provider to ensure safe medication use while breastfeeding. |
Frequently Asked Questions
Is It Safe to Breastfeed After Taking Toradol?
Yes, it's generally safe to breastfeed after taking Toradol. The minimal drug transfer to breast milk makes it a low-risk option. Healthcare providers can offer personalized advice. Consulting them is essential for the best guidance.
What Are the Side Effects of Tramadol While Breastfeeding?
While breastfeeding, tramadol may cause drowsiness or respiratory depression in infants. It's important to monitor babies for signs of excessive sedation. Consult a healthcare provider to weigh the risks and benefits. Always prioritize your baby's well-being.
Which Pain Medication Should Be Avoided in Breastfeeding Mothers?
Avoid ketorolac in breastfeeding. Its potent effects pose risks for nursing infants. Limited data on its transfer to breast milk raises concerns. Opt for safer pain meds postpartum to protect newborns from potential harm.
What Should I Monitor When Taking Toradol?
We monitor signs of gastrointestinal bleeding, pain levels, allergic reactions like rash or swelling, kidney function, and blood pressure while on Toradol. Staying vigilant helps us catch any potential issues early and guarantee safe usage.
Conclusion
To summarize, while Toradol is deemed relatively safe for breastfeeding mothers, caution should be exercised due to its potential impact on milk supply and risks for babies, especially newborns. It's crucial to explore alternatives and consult with a healthcare provider for personalized advice.
Studies have shown that the levels of Toradol in breast milk are usually low with oral dosages, but more research is needed to fully understand its effects on nursing infants.