During our examination of the intricate effects of COVID-19 on pregnancy in the third trimester, we identified various complications that necessitate thoughtful analysis and understanding.
From heightened risks to adjustments in prenatal care, the impact of the virus on expectant parents is profound.
Delving into these 10 key aspects sheds light on the challenges faced by pregnant individuals in these uncertain times, prompting a closer look at the implications for both maternal and fetal health.
Key Takeaways
- Pregnant individuals face heightened risks of severe COVID-19 complications in the third trimester.
- Third-trimester prenatal care involves increased monitoring to safeguard maternal and fetal health.
- Emotional support networks are crucial for alleviating stress and uncertainty during this critical period.
- Navigating labor and delivery concerns, including restrictions and COVID-19 protocols, is essential for a safe experience.
Increased Risk of Complications
Pregnant individuals in the third trimester face a heightened vulnerability to severe complications when contracting COVID-19. The risk of severe illness and ICU admission is greatly increased during this critical stage of pregnancy. Complications such as preterm delivery, stillbirth, and preeclampsia become more probable, posing a serious threat to both the pregnant individual and the developing fetus.
COVID-19 can also impact placental function, further complicating the management of pregnancy in the third trimester. It's imperative to note that vaccinated pregnant individuals exhibit lower risks of complications compared to those who are unvaccinated, emphasizing the importance of vaccination in protecting maternal and fetal health.
Given these risks, managing other health conditions alongside COVID-19 in the third trimester requires a thorough, multidisciplinary approach to ensure the best possible outcomes for both the pregnant person and their baby.
Changes in Prenatal Care Visits

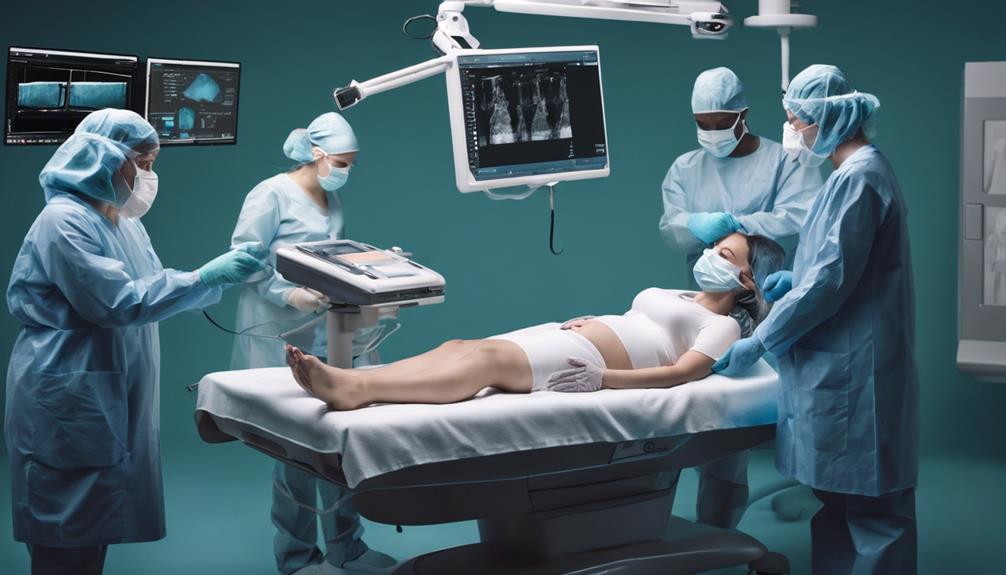
During the third trimester, changes in prenatal care visits may involve increased monitoring of maternal and fetal health to guarantee the best results for both individuals. Health providers may schedule additional ultrasounds and tests during these visits to evaluate the baby's growth, amniotic fluid levels, and placental function. Discussions may focus on preparing for labor, creating birth plans, and addressing any concerns about the impending delivery. Furthermore, healthcare professionals often discuss fetal positioning, signs of labor, and potential complications that could arise in the third trimester to make sure expectant parents are well-informed and prepared for what lies ahead.
As the due date approaches, these visits become vital for monitoring the well-being of both the pregnant individual and the baby.
The increased monitoring aims to facilitate a smooth shift to labor and delivery, ensuring a safe and healthy outcome for both mother and child.
Engaging in open and informative discussions during these visits can help alleviate anxiety and build confidence as labor and delivery draw near.
Emotional Impact on Expectant Parents
In the third trimester, expectant parents often grapple with heightened emotional stress and uncertainty, exacerbated by the challenges posed by the ongoing COVID-19 pandemic. The combination of pregnancy-related concerns and the additional stressors brought about by the pandemic can lead to increased emotional distress and anxiety for soon-to-be parents. Feelings of isolation due to limited support during labor, virtual prenatal classes, and the absence of traditional gatherings like baby showers can further compound these emotions. The fear of contracting COVID-19 before delivery or passing it on to the newborn can greatly escalate anxiety levels in the final stages of pregnancy. It is important for expectant parents to seek emotional support, maintain open communication with healthcare providers, and utilize virtual resources to help alleviate some of the emotional burdens experienced during this critical period.
| Challenges | Coping Strategies |
|---|---|
| Feelings of isolation | Seeking virtual support groups and counseling |
| Fear of COVID-19 exposure | Engaging in relaxation techniques and mindfulness |
| Uncertainty about hospital protocols | Establishing clear communication with healthcare providers |
| Disappointment over canceled in-person events | Creating virtual alternatives for connection |
| Anxiety about virus transmission to the newborn | Following recommended safety guidelines diligently |
Potential Impact on Fetal Development
Maternal COVID-19 infection in the third trimester poses significant risks to fetal development, potentially leading to concerns such as fetal growth restrictions and delays in developmental milestones.
The impact of the virus on the placenta and oxygen supply can affect the baby's brain development, raising worries about cognitive and neurological outcomes.
Exposure to severe COVID-19 during this critical period may trigger inflammatory responses that harm the placenta, ultimately hindering fetal growth and increasing the risk of long-term health implications for the baby.
Fetal Growth Concerns
Concerns about fetal growth in the third trimester of pregnancies affected by COVID-19 arise due to the potential impact of placental insufficiency on the baby's development. Reduced oxygen and nutrient supply to the fetus may result from COVID-19-related placental issues in this critical phase.
Impaired fetal development can occur if the placenta is compromised by COVID-19, affecting the baby's growth and well-being. Monitoring fetal growth through ultrasound scans becomes vital in the third trimester for early detection of any impact from COVID-19.
Fetal growth concerns in this stage due to COVID-19 highlight the necessity of close monitoring and timely interventions to support the best development.
Developmental Milestone Delays
During the critical third trimester of pregnancy, potential delays in fetal developmental milestones can be linked to maternal COVID-19 infection. Factors such as placental insufficiency due to the virus may disrupt nutrient and oxygen supply, impacting fetal growth and neurodevelopment.
The maternal-fetal transmission of COVID-19 can trigger immune system activation, leading to inflammation in the placenta, which in turn can interfere with normal fetal brain development. These disruptions in neurodevelopmental processes during this essential period may result in developmental delays with long-term consequences that are still under investigation.
Understanding the intricate interplay between COVID-19 infection and fetal development is essential for providing thorough care to pregnant individuals facing these challenges.
Concerns About Labor and Delivery

As we navigate the challenges of labor and delivery during the third trimester amidst the COVID-19 pandemic, ensuring thorough symptom screening remains paramount for safeguarding maternal and fetal health. Concerns about labor induction due to maternal infection risks, limitations on support people, and the need for continuous symptom screening weigh heavily on expectant mothers. The uncertainty of potential separation from the newborn in cases of severe maternal illness adds a layer of emotional distress to an already complex situation. Immediate testing and medical treatment upon COVID-19 exposure become critical decisions to protect both the mother and the baby during this vulnerable period.
The fear of labor induction due to COVID-19 risks can be overwhelming for expectant mothers.
Restrictions on the number of support people during labor can lead to feelings of isolation and anxiety.
The possibility of being separated from the newborn due to illness can evoke deep emotional turmoil for mothers in the third trimester.
Managing Stress and Anxiety

Handling the challenges of the third trimester amidst the COVID-19 pandemic, managing stress and anxiety becomes essential for safeguarding maternal and fetal well-being. Pregnant women in their third trimester are particularly vulnerable to increased anxiety, which can have detrimental effects on pregnancy. It is important to employ stress management techniques such as mindfulness, relaxation exercises, and counseling to alleviate these anxieties. Persistent stress and anxiety during this critical period can impact prenatal development and birth outcomes, underscoring the importance of seeking support from healthcare providers, therapists, and support groups.
| Stress Management Techniques | Benefits |
|---|---|
| Mindfulness | Reduces anxiety levels |
| Relaxation exercises | Promotes calmness |
| Counseling | Provides emotional support |
| Support groups | Offers shared experiences |
Incorporating these strategies can not only help pregnant individuals navigate the uncertainties of the third trimester but also contribute to better maternal health outcomes. Healthcare providers play an important role in supporting pregnant women with COVID-related stress and anxiety, ensuring a holistic approach to maternal care.
Impact on Support Systems

In handling the challenges of the third trimester, establishing robust support systems is essential for ensuring the well-being of pregnant individuals. During this critical phase, the impact of support systems can't be overstated.
Here are three key elements that highlight the importance of support systems for pregnant individuals in the third trimester:
- Emotional Support: Providing a listening ear, empathy, and understanding can help alleviate stress, anxiety, and uncertainties that often accompany the final stages of pregnancy. Feeling emotionally supported can notably impact the mental well-being of pregnant individuals.
- Practical Assistance: Assistance with daily tasks such as household chores, meal preparation, and childcare for other children can ease the physical burden on pregnant individuals. Having practical help allows them to focus on their health and preparing for the arrival of their baby.
- Reliable Information: Access to accurate and reliable information about labor, delivery, and postpartum care is crucial for pregnant individuals. Knowing what to expect and being well-informed can help them feel more confident and prepared as they approach childbirth.
Building a strong support network that encompasses emotional support, practical assistance, and reliable information is vital for pregnant individuals in the third trimester. It can enhance their overall well-being, reduce feelings of isolation, and contribute to a positive pregnancy experience.
Preparing for a COVID-19 Positive Diagnosis

Preparation for a positive COVID-19 diagnosis during the third trimester of pregnancy is a critical aspect of ensuring the well-being of both the pregnant individual and the baby. If experiencing symptoms or exposed to COVID-19, contacting healthcare providers promptly is crucial for receiving appropriate guidance. Monitoring symptoms closely and following healthcare provider recommendations for managing COVID-19 at home can help prevent complications. Ensuring adequate rest, hydration, and nutrition while isolating at home supports recovery and minimizes the impact of COVID-19 on the pregnancy. Being prepared with emergency contacts, healthcare providers, and essential medications can expedite response and treatment in case of worsening symptoms or emergencies.
| Action | Importance | Benefit |
|---|---|---|
| Contacting Providers | Prompt response | Receive guidance and appropriate care |
| Monitoring Symptoms | Close observation | Prevent complications |
| Rest, Hydration, Nutrition | Essential care | Support recovery and minimize impact |
Navigating Hospital Policies and Restrictions

How do hospitals manage support persons and visitor restrictions during labor and delivery amidst the COVID-19 pandemic? Hospital policies are adapting to prioritize the safety of all individuals involved in the pregnancy journey.
Here are three key points essential for taking into account:
- Limited Support Persons: Hospitals have restrictions on the number of support persons allowed during labor, which can impact the emotional support available to the pregnant individual.
- COVID-19 Testing: Some hospitals mandate COVID-19 testing upon admission for labor and delivery to create a secure environment for both patients and healthcare providers.
- Visitor Restrictions: Postpartum care may be affected by visitor limitations, making it vital for families to plan alternative ways to receive support during this delicate phase.
Understanding and complying with these hospital policies are vital for a smooth experience in the third trimester, ensuring a safe and supportive environment for both the pregnant person and their newborn.
Postpartum Challenges and Adjustments
Handling the physical and emotional challenges that come with the postpartum period in the third trimester requires a blend of resilience and adaptability. Physical recovery from labor and delivery, hormonal changes, and the risk of postpartum depression are significant factors during this time.
Women in the third trimester might find themselves struggling with fatigue, weight loss concerns, and the demands of new responsibilities. Adjustments may be necessary for breastfeeding, sleep schedules, and managing postpartum emotions effectively.
The heightened risk of postpartum depression in the third trimester is often attributed to hormonal shifts and the overwhelming nature of newfound duties. To navigate these challenges successfully, support systems and self-care practices play an important role.
Seeking assistance and implementing self-compassion strategies can aid in overcoming the hurdles associated with postpartum challenges, ensuring a smoother change into this phase of pregnancy.
Frequently Asked Questions
Does COVID Affect Baby in Third Trimester?
Yes, COVID can impact the baby in the third trimester. It may lead to growth issues, preterm birth, and fetal distress. Maternal infection affects placental function, potentially harming the baby. Neonatal complications and adverse outcomes for both mother and baby are concerning.
What Are the Complications of Getting COVID While Pregnant?
Experiencing COVID-19 during pregnancy raises risks like severe illness, preterm delivery, and challenges in managing other health conditions. Vaccination in the third trimester reduces these risks, emphasizing the importance of protection for both mother and baby.
How Does COVID-19 Affect the Outcomes of Pregnancy?
COVID-19 can impact pregnancy outcomes markedly. It may lead to preterm birth, neonatal distress, and the need for cesarean delivery. Severe cases could require timely delivery for maternal and fetal well-being, sometimes necessitating antenatal corticosteroids for lung maturation.
What Are the Long Term Effects of COVID-19 on Pregnancy?
We acknowledge the importance of understanding the long-term effects of COVID-19 on pregnancy. Research suggests potential risks such as preterm birth, stillbirth, and neurodevelopmental issues. Ongoing studies are essential for optimizing maternal and child health outcomes.
Conclusion
To summarize, addressing the challenges of COVID-19 during the third trimester of pregnancy demands careful consideration and proactive measures.
As we progress through this crucial stage, let's recall that we aren't alone in confronting these uncertainties. Together, we can withstand the storm and emerge stronger, like a beacon of hope in the midst of a turbulent sea.
Stay informed, stay connected, and stay vigilant for the well-being of both mother and child.









